Oops + Hi Dr. Sam - it was the antipsychotic Chlorpromazine - also known as Thorazine - that was derived from reserpine a chemical found in Indian Snake Root - Rauwolfia serpetina
And seqchem.com says the LD 50 for Risperidone was "LD50: ~30 (mg/kg) iv in mice" [6th headline up from bottom of Website under: "Toxological Information"]
Definition of "LD 50" from Merriam Webster's Online Dictionary
Wiki says Cathars were veggies [scroll 1/3 way down to "Social Relationships"] because they thought animals might contain reincarnated...
Genesis 1:29 says God gave us seed bearing vegetation to eat.
Genesis 1:26 says God gave us "dominion" over animals, fish + birds.
Genesis 6: 5 - 7 says God grew sad at all the badness in men's hearts before deciding to drown us.
Wiki says almost all the world's faiths have a version of Matthew 7: 12
Genesis 3:20 says God made clothes out of apparently available dead animal skins after Adam + Eve ate whatever they ate to lose eternal life, which it is left unclear whether the animals also enjoyed before the "original bite"
Genesis 4 says Abel was killed by Cain after he had offered the fat of his first born sheep to God while Cain, who survived to be rebooted out of wherever they were, offered some vegetation.
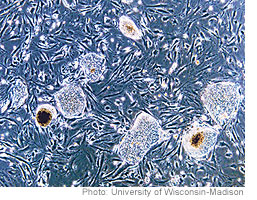
PETA list of successful alternatives to animal testing such as VaxDesign's dime sized human immune system made with human cells grown in vitro, and curiously, the use of transcranial magnetic stimulation to "temporarily and reversibly induce brain disorders" HUH?
temporarily and reversibly induce brain disorders using transcranial magnetic stimulation.
Genesis 1:26 says God gave us "dominion" over animals, fish + birds.
Genesis 6: 5 - 7 says God grew sad at all the badness in men's hearts before deciding to drown us.
Wiki says almost all the world's faiths have a version of Matthew 7: 12
Genesis 3:20 says God made clothes out of apparently available dead animal skins after Adam + Eve ate whatever they ate to lose eternal life, which it is left unclear whether the animals also enjoyed before the "original bite"
Genesis 4 says Abel was killed by Cain after he had offered the fat of his first born sheep to God while Cain, who survived to be rebooted out of wherever they were, offered some vegetation.
PETA list of successful alternatives to animal testing such as VaxDesign's dime sized human immune system made with human cells grown in vitro, and curiously, the use of transcranial magnetic stimulation to "temporarily and reversibly induce brain disorders" HUH?
temporarily and reversibly induce brain disorders using transcranial magnetic stimulation.
CBS News says study finds veggie diet lowers cholesterol - actual study here
NPR says study found red meat eaters had 13% higher risk of mortality + 20% higher risk of cancer, heart disease deaths. Study found here
NPR says study found red meat eaters had 13% higher risk of mortality + 20% higher risk of cancer, heart disease deaths. Study found here
Atherotech Diagnostics Lab says they are the only lab to perform the VAP cholesterol test and that the VAP Test was clinically tested on humans and animals..
http://en.wikipedia.org/wiki/Antipsychotic says in the 8th paragraph:
Schizophrenia
"In people with schizophrenia less than half (41%) showed any therapeutic response to an atypical antipsychotic, compared to 24% on placebo, there is a decline in treatment response over time, and potentially a biases in the literature in favor of these medication.[7] Risperidone (an atypical antipsychotic), shows only marginal benefit compared with placebo and that, despite its widespread use, evidence remains limited, poorly reported and probably biased in favor of risperidone due to pharmaceutical company funding of trials.[8]"
[8] ^ Rattehalli RD, Jayaram MB, Smith M (2010). "Risperidone versus placebo for schizophrenia". Cochrane Database Syst Rev (1): CD006918. doi:10.1002/14651858.CD006918. PMID 20091611.
http://en.wikipedia.org/wiki/Risperidone
http://www.rxlist.com/risperdal-drug.htm Says:
"RISPERDAL® contains risperidone, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. The chemical designation is 3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)- 1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C23H27FN4O2 and its molecular weight is 410.49. The structural formula is:
[8] ^ Rattehalli RD, Jayaram MB, Smith M (2010). "Risperidone versus placebo for schizophrenia". Cochrane Database Syst Rev (1): CD006918. doi:10.1002/14651858.CD006918. PMID 20091611.
http://en.wikipedia.org/wiki/Risperidone
http://www.rxlist.com/risperdal-drug.htm Says:
"RISPERDAL® contains risperidone, an atypical antipsychotic belonging to the chemical class of benzisoxazole derivatives. The chemical designation is 3-[2-[4-(6-fluoro-1,2-benzisoxazol-3-yl)- 1-piperidinyl]ethyl]-6,7,8,9-tetrahydro-2-methyl-4H-pyrido[1,2-a]pyrimidin-4-one. Its molecular formula is C23H27FN4O2 and its molecular weight is 410.49. The structural formula is:
 |
.
"RISPERDAL® Tablets are for oral administration and available in 0.25 mg (dark yellow), 0.5 mg (red-brown), 1 mg (white), 2 mg (orange), 3 mg (yellow), and 4 mg (green) strengths. RISPERDAL® tablets contain the following inactive ingredients: colloidal silicon dioxide, hypromellose, lactose, magnesium stearate, microcrystalline cellulose, propylene glycol, sodium lauryl sulfate, and starch (corn). The 0.25 mg, 0.5 mg, 2 mg, 3 mg, and 4 mg tablets also contain talc and titanium dioxide. The 0.25 mg tablets contain yellow iron oxide; the 0.5 mg tablets contain red iron oxide; the 2 mg tablets contain FD&C Yellow No. 6 Aluminum Lake; the 3 mg and 4 mg tablets contain D&C Yellow No. 10; the 4 mg tablets contain FD&C Blue No. 2 Aluminum Lake.
RISPERDAL® is also available as a 1 mg/mL oral solution. RISPERDAL® Oral Solution contains the following inactive ingredients: tartaric acid, benzoic acid, sodium hydroxide, and purified water.
RISPERDAL® M-TAB® Orally Disintegrating Tablets are available in 0.5 mg (light coral), 1 mg (light coral), 2 mg (coral), 3 mg (coral), and 4 mg (coral) strengths. RISPERDAL® M-TAB® Orally Disintegrating Tablets contain the following inactive ingredients: Amberlite® resin, gelatin, mannitol, glycine, simethicone, carbomer, sodium hydroxide, aspartame, red ferric oxide, and peppermint oil. In addition, the 2 mg, 3 mg, and 4 mg RISPERDAL® M-TAB® Orally Disintegrating Tablets contain xanthan gum."
````````````````````````````````````````````````````````````````````````
http://www.schizophrenia.com/treatments.php# :
"Complementary Schizophrenia Treatments - Table of Contents
- Schizophrenia Treatments that Have Shown Some Benefits in Scientific Testing
- Possible Schizophrenia Treatments that have shown some early positive results in studies
- Future Potential Therapies
- Disproven (or Unproven) & Overmarketed "Schizophrenia Treatments"
please remember that niacin cures pellegra
http://jungcircle.com/schiznatural.htm
http://www.schizophrenia.com/treatments.php
http://en.wikipedia.org/wiki/Reserpine:
"Reserpine was isolated in 1952 from the dried root of Rauwolfia serpentina (Indian snakeroot),[4] which had been known as Sarpagandha and had been used for centuries in India for the treatment of insanity, as well as fever and snakebites[1] — even Mahatma Gandhi used it as a tranquilizer.[6] It was first used in the United States by Robert Wallace Wilkins in 1950. Its molecular structure was elucidated in 1953 and natural configuration published in 1955.[7] It was introduced in 1954, two years after chlorpromazine.[5] The first total synthesis was accomplished by R. B. Woodward in 1958"[7]
 http://photos.merinews.com/newPhotoLanding.jsp?imageID=14838
http://photos.merinews.com/newPhotoLanding.jsp?imageID=14838
Indian Snakeroot
http://www.motherherbs.com/rauwolfia-serpentina.html
Indian Snakeroot flower

http://jungcircle.com/schiznatural.htm
http://www.schizophrenia.com/treatments.php
http://en.wikipedia.org/wiki/Reserpine:
"Reserpine was isolated in 1952 from the dried root of Rauwolfia serpentina (Indian snakeroot),[4] which had been known as Sarpagandha and had been used for centuries in India for the treatment of insanity, as well as fever and snakebites[1] — even Mahatma Gandhi used it as a tranquilizer.[6] It was first used in the United States by Robert Wallace Wilkins in 1950. Its molecular structure was elucidated in 1953 and natural configuration published in 1955.[7] It was introduced in 1954, two years after chlorpromazine.[5] The first total synthesis was accomplished by R. B. Woodward in 1958"[7]
 http://photos.merinews.com/newPhotoLanding.jsp?imageID=14838
http://photos.merinews.com/newPhotoLanding.jsp?imageID=14838Indian Snakeroot

http://www.motherherbs.com/rauwolfia-serpentina.html
Indian Snakeroot flower

| Systematic (IUPAC) name | |
|---|---|
| Methyl (3β,16β,17α,18β,20α)-11,17-dimethoxy-18-[(3,4,5-trimethoxybenzoyl)oxy]yohimban-16-carboxylate |
http://en.wikipedia.org/wiki/Antipsychotic Wikipedia list of antipsychotics [scroll to middle of page]:
First-generation antipsychotics
Main article: Typical antipsychotic
Butyrophenones
Main article: Butyrophenones
- Haloperidol (Haldol, Serenace)
- Droperidol (Droleptan, Inapsine)
Phenothiazines
Main article: Phenothiazines
- Chlorpromazine (Thorazine, Largactil)
- Fluphenazine (Prolixin) – Available in decanoate (long-acting) form
- Perphenazine (Trilafon)
- Prochlorperazine (Compazine)
- Thioridazine (Mellaril)
- Trifluoperazine (Stelazine)
- Mesoridazine (Serentil)
- Periciazine
- Promazine
- Triflupromazine (Vesprin)
- Levomepromazine (Nozinan)
- Promethazine (Phenergan)
- Pimozide (Orap)
- Cyamemazine (Tercian)
Thioxanthenes
Main article: Thioxanthenes
- Chlorprothixene (Cloxan, Taractan, Truxal)
- Clopenthixol (Sordinol)
- Flupenthixol (Depixol, Fluanxol)
- Thiothixene (Navane)
- Zuclopenthixol (Cisordinol, Clopixol, Acuphase)
Second-generation antipsychotics[edit]
Main article: Atypical antipsychotic
- Clozapine (Clozaril) – Requires complete blood counts every one to four weeks due to the risk of agranulocytosis.
- Olanzapine (Zyprexa) – Used to treat psychotic disorders including schizophrenia, acute manic episodes, and maintenance of bipolar disorder
- Risperidone (Risperdal) – Divided dosing is recommended until initial titration is completed, at which time the drug can be administered once daily. Used off-label to treat Tourette syndrome and anxiety disorder.
- Quetiapine (Seroquel) – Used primarily to treat bipolar disorder and schizophrenia.
- Ziprasidone (Geodon) – Approved in 2004[82] to treat bipolar disorder. Side-effects include a prolonged QT interval in the heart, which can be dangerous for patients with heart disease or those taking other drugs that prolong the QT interval.
- Amisulpride (Solian) – Selective dopamine antagonist. Higher doses (greater than 400 mg) act upon post-synaptic dopamine receptors resulting in a reduction in the positive symptoms of schizophrenia, such as psychosis. Lower doses, however, act upon dopamine autoreceptors, resulting in increased dopamine transmission, improving the negative symptoms of schizophrenia. Lower doses of amisulpride have also been shown to have antidepressant and anxiolytic effects in non-schizophrenic patients, leading to its use in dysthymia and social phobias. Amisulpride has not been approved for use by the Food and Drug Administration in the United States.
- Asenapine (Saphris) is a 5-HT2A- and D2-receptor antagonist developed for the treatment of schizophrenia and acute mania associated with bipolar disorder.
- Paliperidone (Invega) – Derivative of risperidone that was approved in 2006, it offers a controlled release once-daily dose, or a once-monthly depot injection.
- Iloperidone (Fanapt, Fanapta, and previously known as Zomaril) – Approved by the FDA in 2009, it is fairly well tolerated, although hypotension, dizziness, and somnolence were very common side effects.
- Zotepine (Nipolept, Losizopilon, Lodopin, Setous) – An atypical antipsychotic indicated for acute and chronic schizophrenia. It was approved in Japan circa 1982 and Germany in 1990.
- Sertindole (Serdolect, and Serlect in Mexico). Sertindole was developed by the Danish pharmaceutical company H. Lundbeck. Like the other atypical antipsychotics, it is believed to have antagonist activity at dopamine and serotonin receptors in the brain.
- Lurasidone (Latuda), recently approved by the FDA for schizophrenia and pending approval for bipolar disorder. Given once daily, it has shown mixed Phase III efficacy results but has a relatively well-tolerated side effect profile.
Third-generation antipsychotics[edit]
- Aripiprazole (Abilify) – Mechanism of action is thought to reduce susceptibility to metabolic symptoms seen in some other atypical antipsychotics.[83]
Mechanism of action[edit]
http://brainblogger.com/2012/05/29/full-recovery-from-schizophrenia/
http://brainblogger.com/2012/05/29/full-recovery-from-schizophrenia/
http://overcomingschizophrenia.blogspot.com/
http://schizophreniasucks.blogspot.com/
http://schizophrenia-blog.blogspot.com/
http://mindriddles.blogspot.com/
 |  |
| Home | About | Donate/Volunteer | Contact | |
| Schizophrenia Information > Complementary Treatments | |||||||||||||
Complementary Schizophrenia Treatments | |||||||||||||
Important Warning: The following web page is provided for information purposes only. It covers possible complementary treatment approaches that may be used in concert with antipsychotic (neuroleptic) medications. The adoption of any of these complementary treatments should be done with a qualified psychiatrist or psychologist's knowledge and approval as part of a person's complete treatment plan. This summary of possible complementary treatments is for informational purposes only.
Cognitive Behavioral Therapy (CBT) has been judged by the Cochrane review as potentially positive for people with schizophrenia, stating that evidence suggests " that it [CBT] may well be of value, at least in the short term. Cognitive behavioural therapy should be further evaluated in various clinical settings and comparing effects for both expert and less skilled practitioners." Source; Cochrane Review Family therapy and assertive community treatment have clear effects on the prevention of psychotic relapse and rehospitalization. However, these treatments have no consistent effects on other outcome measures (e.g., pervasive positive and negative symptoms, overall social functioning, and ability to obtain competitive employment). Social skills training improves social skills but has no clear effects on relapse prevention, psychopathology, or employment status. Supportive employment programs that use the place-and-train vocational model have important effects on obtaining competitive employment. Some studies have shown improvements in delusions and hallucinations following cognitive behavior therapy. Preliminary research indicates that personal therapy may improve social functioning. Research suggests that relatively simple, long-term psychoeducational family therapy should be available to the majority of persons suffering from schizophrenia. Assertive community training programs ought to be offered to patients with frequent relapses and hospitalizations, especially if they have limited family support. Patients with schizophrenia can clearly improve their social competence with social skills training, which may translate into a more adaptive functioning in the community. For patients interested in working, rapid placement with ongoing support offers the best opportunity for maintaining a regular job in the community. Cognitive behavior therapy may benefit the large number of patients who continue to experience disabling psychotic symptoms despite optimal pharmacological treatment. (Source - psychosocial treatment, 2001 - see below) Glycine (an amino acid sold as a dietary supplement) has been a subject of research for over 15 years as a potential treatment for the negative symptoms of schizophrenia. Only a handful of human clinical trials with fewer than 50 people in each trial, have been completed (though one trial with 150 people has recently completed and has not yet been published). The trials published to date are reporting that the results have been quite positive, showing a significant reduction (averaging around 24%) in negative and cognitive symptoms based on the PANSS (Positive and Negative Schizophrenia Symptoms) scale. The clinical trials have shown that Glycine did not help people who are taking Clozapine, but it did help (in reducing negative symptoms) in people who were taking risperidone (Risperdal), and olanzapine (Zyprexa). The clinical trials suggest that the optimal dosage may be in the range of 30 grams to 60 grams a day. The biggest downside to taking glycine seems to be upset stomach and nausea which, researchers tell us, is quite common in people who take 60 grams of glycine a day for a month or two. Approaches used by the researchers to minimize this problem have been to start at lower doses (e.g. 5 to 10 grams split into two doses per day) and then to slowly phase up to higher doses over a period of weeks. Also - taking it after meals may assist in reducing side effects. One hypothesis of schizophrenia pathology suggests that NMDA-receptor disfunction (a special kind of glutamate receptor in the brain) may contribute to disordered synapses and brain atrophy, which ultimately result in the visible symptoms. Glycine may turn out to be a very beneficial supplemental treatment (when added to standard antipsychotic medications) for some people with schizophrenia. We hope to see longer and larger trials for glycine supplemental treatments. Talk with your doctor if you think you may benefit (review the report below for information on what glycine does and who it might help). See special report below for more information:
One reliable provider we are familiar in the USA and that we've had good experiences with is the Internet-store www.iherb.com - and specifically products from the "NOW Foods" company. Other leading companies that are known to have good manufacturing quality processes include Twinlab. We have no affiliation with either of these organizations. (Please note that there are no studies the schizophrenia researchers we are in contact with are aware of that support the idea that any type of vitamin or fatty acid (EFA) will cure schizophrenia. There are currently no cures for schizophrenia.) Supporting Research (a sample):
Music Therapy - Music therapy is a type of psychotherapy in which the patient is encouraged to utilize music to improve interpersonal and communication skills in ways that regular dialogue is limited. Forms of music therapy generally are based around cognitive/behavioral, humanistic or psychoanalytic frameworks or a mixture of approaches. There are usually both active and receptive parts of the therapy, meaning that at times music is listened to and at other times there is the use of musical improvisation or creation. There have not been many studies on music therapy and schizophrenia, but the Cochrane review looked at the data available for a recent review. There were 4 studies included in the review. These studies looked at short term benefits of music therapy when used in addition to more conventional pharmaceutical treatments. The authors combined the results of these 4 studies in a “meta-analysis” meaning that the studies were similar enough that the data could be combined and form a larger sample. The number of sessions used in these studies varied from 7 to 75 and the length of time studied ranged up to 3 months duration. The results were encouraging. In one study, it was shown that the global state in the short term was frequently improved. Using a statistic called “number needed to treat (NNT)” it was described that to show an improvement in one patient, you only needed to put two patients through the therapy. (This compares with NNT in many situations of several hundred patients needed to be given a treatment in order to notice benefits in one person.) It was shown that the number of sessions had a direct impact on the success of the treatment with more sessions being better. It was also seen that active participation was better than a more passive approach to treatment. However, the length of treatment in theses studies was short and the benefit in the long term was unknown. Tharyan P, Adams C. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev. 2005 Apr 18;(2):CD000076. Click here for article 1 on PubMed Gold C, Heldal T, Dahle T, Wigram T. Music therapy for schizophrenia or schizophrenia-like illnesses. Cochrane Database Syst Rev. 2005 Apr 18;(2):CD004025. Click here for article 2 on PubMed Simpling listening to music listening may also, however, be useful as a means of relaxation or group discussion stimulus. A medical review article (April 2005) has indicated that music therapy may be beneficial for people already on a standard treatment for schizophrenia. Music therapy should in no way replace a standard treatment regimen. Future research may reveal more positive results.
In January, 2006 The Cochrane Review (a leading medical publisher) published a review article of all the studies that have been done so far on chinese herbal medicine use in treatment for schizophrenia. In their review article they stated: "Traditional Chinese medicine (TCM) has been used to treat mental health disorders, including schizophrenia, for more than 2000 years. Chinese herbs may also have antipsychotic properties when used in a Western biomedical context. In this review we sought and found trials relevant to the effects of both approaches for schizophrenia. Traditional Chinese medicine methodology has been evaluated for schizophrenia, but the one included study was too limited in terms of sample size and study length to guide good practice. However, this pioneering study does show that TCM can be evaluated for its efficacy for people with schizophrenia , and should encourage trialists to undertake further, more comprehensive trials in this area.Future Potential Therapies
Vitamin B6 - Vitamin B6 has also in the past been claimed to be a "cure" for schizophrenia (wrongly, as the data below indicates). As you should expect by now - if anyone makes any claims about a cure for schizophrenia - ask for some 3rd party validation studies from the major schizophrenia research centers around the world. Relevant Information and Research: Relevant Information and Research: Art Therapy for Schizophrenia The Cochrane Review (a leading medical review publication) has this to say about Art Therapy for Schizophrenia. |
This site does not provide medical or any other health care or fitness advice, diagnosis, or treatment. The site and its services, including the information above, are for informational purposes only and are not a substitute for professional medical or health advice, examination, diagnosis, or treatment. Always seek the advice of your physician or other qualified health professional before starting any new treatment, making any changes to existing treatment, or altering in any way your current exercise or diet regimen. Do not delay seeking or disregard medical advice based on information on this site. Medical information changes rapidly and while Schizophrenia.com makes efforts to update the content on the site, some information may be out of date. No health information on Schizophrenia.com, including information about herbal therapies and other dietary supplements, is regulated or evaluated by the Food and Drug Administration and therefore the information should not be used to diagnose, treat, cure, or prevent any disease without the supervision of a medical doctor.
|
Subscribe to: Posts (Atom)
Blog Archive
http://jama.jamanetwork.com/article.aspx?articleid=1104262
http://www.cbsnews.com/8301-504763_162-20096551-10391704/cholesterol-lowering-foods-better-than-low-fat-diet-what-study-says/
http://www.atherotech.com/vapcholtest/researchers.asp
http://archinte.jamanetwork.com/article.aspx?articleid=1134845
Death By Bacon? Study Finds Eating Meat Is Risky : The Salt : NPR :
"He found that people who consumed about one serving of red meat (beef, pork or lamb) per day had a 13 percent increased risk of mortality, compared with those who were eating very little meat. And processed meats raised the risk higher, to about a 20 percent increased risk of death from diseases including cancer and heart disease."
http://www.cbsnews.com/8301-504763_162-20096551-10391704/cholesterol-lowering-foods-better-than-low-fat-diet-what-study-says/
http://www.atherotech.com/vapcholtest/researchers.asp
http://archinte.jamanetwork.com/article.aspx?articleid=1134845
Death By Bacon? Study Finds Eating Meat Is Risky : The Salt : NPR :
"He found that people who consumed about one serving of red meat (beef, pork or lamb) per day had a 13 percent increased risk of mortality, compared with those who were eating very little meat. And processed meats raised the risk higher, to about a 20 percent increased risk of death from diseases including cancer and heart disease."

If you share a kitchen with non-dieters, store phen 375indulgent foods out of sight.
ReplyDelete